Estrogen and Rosacea: Uncovering the Hormonal Link in Skin Inflammation
For years, rosacea has been considered a condition rooted in inflammation, vascular instability, and microbial imbalance. But now, new research is pointing toward a surprising contributor in its development and severity: estrogen.
Hormonal influences have long been suspected in skin disorders, but rosacea has often been overlooked in this area—until now. Recent studies are exploring how fluctuating estrogen levels may play a key role in the pathogenesis of rosacea, especially in women.
🌸 The Estrogen Connection: What New Research Shows
Recent findings published in dermatology journals and highlighted by Dermatology Times suggest that estrogen may play a significant role in rosacea's development and severity, particularly in the following ways:
1. Estrogen Modulates Inflammation
Estrogen interacts with various immune cells and cytokines, which are responsible for regulating inflammation. In rosacea, where immune responses are already heightened, fluctuations in estrogen may further amplify inflammatory pathways, leading to more frequent or severe flare-ups.
2. Estrogen Affects Blood Vessel Reactivity
One hallmark of rosacea is facial flushing and visible blood vessels, tied to vascular instability. Estrogen is known to influence vasodilation and capillary permeability, meaning that high or fluctuating estrogen levels may increase skin sensitivity to heat, alcohol, or stress, all common rosacea triggers.
3. Menopause and Hormonal Fluctuations
Many women report worsening rosacea symptoms during perimenopause and menopause, which are marked by declining estrogen. This suggests that lower estrogen may also impair skin barrier function, increasing susceptibility to irritation and dryness—both key challenges for rosacea-prone individuals.
🧠 Why This Research Matters
Understanding estrogen’s role in rosacea pathogenesis:
-
May explain why rosacea is more common in women, especially those over 30
-
Opens the door for hormone-related therapies or support strategies, such as hormonal balancing or phytoestrogen-rich skincare
-
Reinforces the importance of tailored skincare approaches during life stages like pregnancy, menopause, or postpartum
🌿 What Can You Do If You Suspect a Hormonal Component?
While more clinical studies are needed, here are some ways to support hormone and skin balance naturally:
-
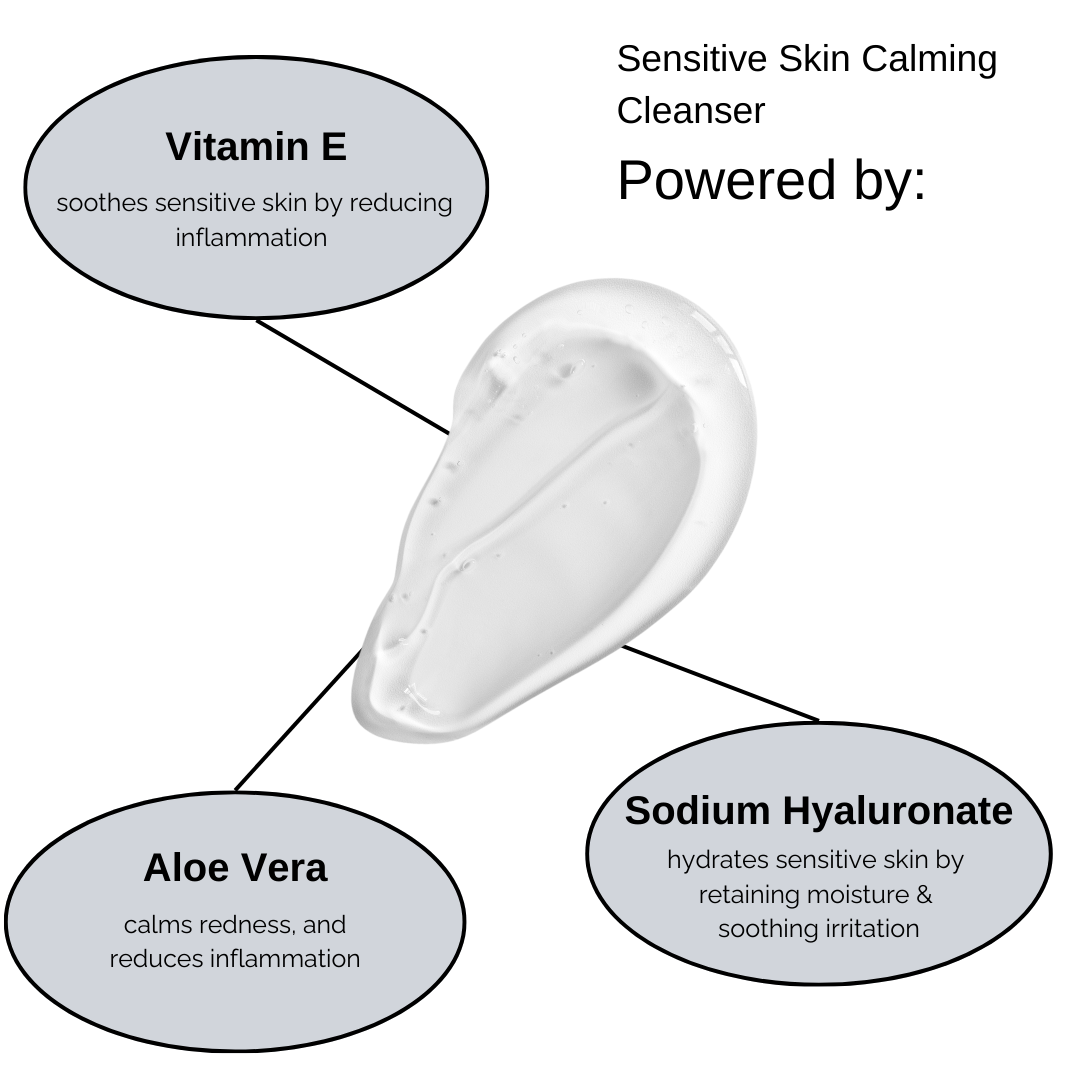
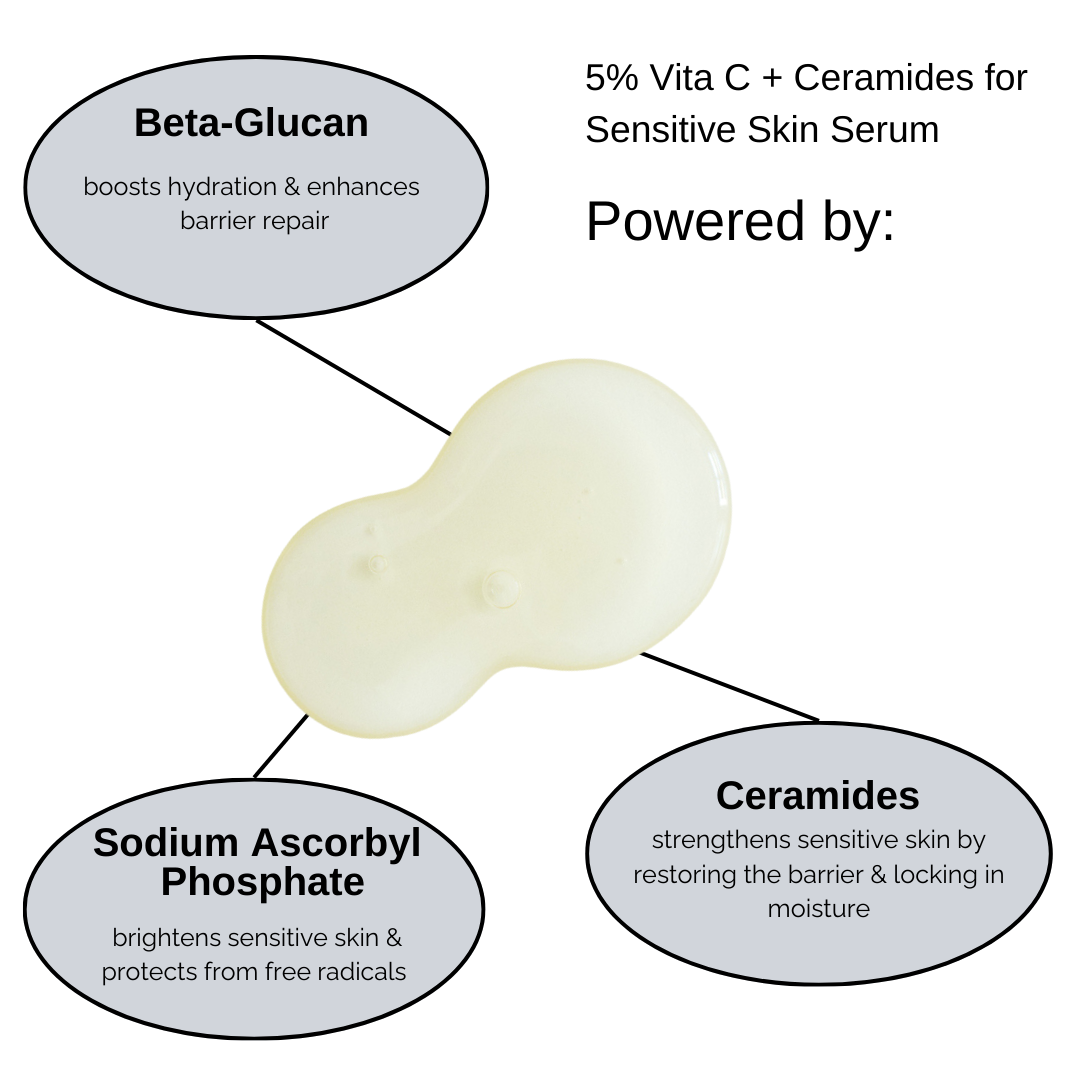
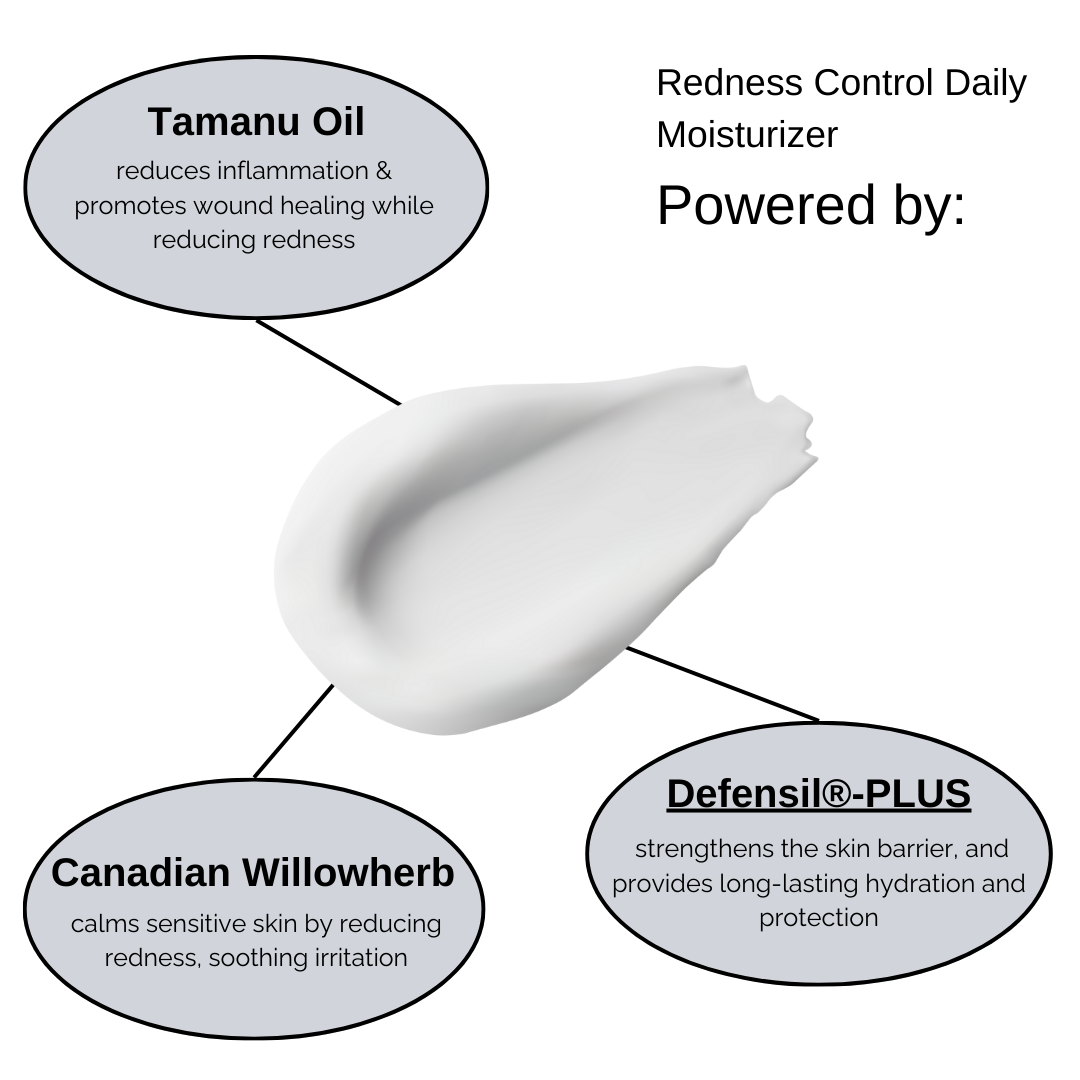
Support your skin barrier: Use rosacea-friendly skincare that hydrates and calms inflammation (like niacinamide, azelaic acid, or centella asiatica).
-
Limit vasodilating triggers: Avoid hot beverages, spicy foods, and extreme temperatures during hormone-sensitive periods.
-
Talk to your healthcare provider: If you notice flares linked to your cycle or menopause, a doctor may recommend hormone testing or supportive therapies.
-
Consider adaptogens or phytoestrogens: Supplements like maca, black cohosh, or soy isoflavones may help support estrogen balance (always check with a professional first).
As research continues to uncover the hormonal link in rosacea, it’s clear that skin health goes deeper than the surface.