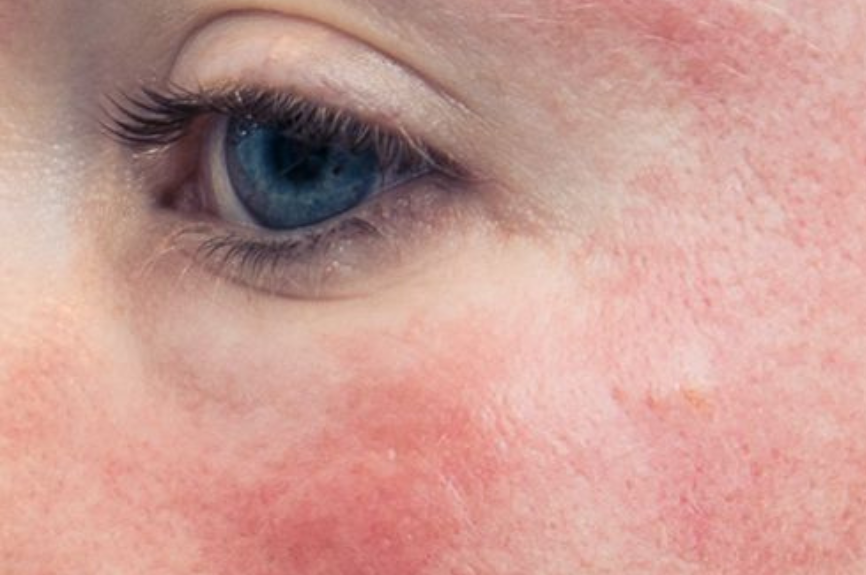
What Causes Rosacea? A Deep Dive into the Science Behind the Redness
Despite decades of research, there’s no single answer. Instead, rosacea is the result of multiple overlapping systems gone awry—inflammation, microbial imbalance, neurovascular dysfunction, and even hormonal fluctuations. In this post, we break down the science behind rosacea’s potential causes and how this knowledge is leading to better care.
1. Immune System Dysfunction
One of the most consistent findings in rosacea research is overactivation of the innate immune system—your body’s first line of defense.
Key Mechanisms:
• Toll-Like Receptor 2 (TLR2) is overexpressed in rosacea skin. This receptor triggers the release of:
• Toll-Like Receptor 2 (TLR2) is overexpressed in rosacea skin. This receptor triggers the release of:
• Cathelicidin (LL-37), an antimicrobial peptide that, in excess, causes inflammation, redness, and blood vessel growth.
• LL-37 also activates the mTOR and JAK-STAT signaling pathways, both of which are associated with inflammation and angiogenesis (new blood vessel formation) in rosacea.
This explains why even minor stimuli—like sun exposure or spicy food—can cause exaggerated responses in rosacea-prone skin.
2. Microbial Imbalance (Especially Demodex Mites)
Rosacea-prone skin often shows an overpopulation of Demodex folliculorum, a microscopic mite that lives in hair follicles.
Why It Matters:
• Demodex mites carry bacteria that may stimulate immune responses and inflammation.
• Recent studies show that treating Demodex overgrowth (e.g., with ivermectin) not only reduces inflammation but also improves the balance of the skin microbiome—increasing beneficial bacteria like Staphylococcus epidermis.
This suggests that rosacea may be partly triggered by an imbalance in the skin’s ecosystem, not just the presence of mites alone.
3. Neurovascular Dysregulation
Rosacea is known for flushing and visible blood vessels, which may be due to abnormal nerve signaling.
Emerging Insights:
• Mast cells, part of the immune system, are highly activated in rosacea and respond to nerve signals.
• New research has shown that modulating glutamate signaling—a nerve communication molecule—can calm mast cells and reduce flushing.
• This means rosacea may involve a kind of neurogenic inflammation, where nerves provoke inflammation in the skin.
4. Hormonal Influences
Hormones also appear to play a role—especially in women.
Key Findings:
• Perimenopause and menopause can worsen rosacea, likely due to reduced estrogen levels, which normally help maintain skin barrier function and control inflammation.
• A 2024 study found that women using hormonal IUDs had higher rates of rosacea compared to those using non-hormonal birth control methods.
These hormonal shifts may not be direct causes but could exacerbate underlying inflammation and vascular reactivity in the skin.
5. Genetic and Autoimmune Links
While rosacea isn’t directly inherited, genetic predispositions may make some people more susceptible.
Research Highlights:
• Genome-wide studies have identified shared genetic markers between rosacea and autoimmune conditions like type 1 diabetes and rheumatoid arthritis.
• Individuals with a family history of rosacea or autoimmune diseases may be more prone to inflammatory overreaction in the skin.
This supports the idea that rosacea is not just a surface-level issue, but tied to deeper systemic imbalances.
6. Environmental and Lifestyle Triggers
While not causes in themselves, certain triggers can activate or worsen rosacea in predisposed individuals:
• UV radiation
• Heat or cold exposure
• Alcohol (especially red wine)
• Stress
• Spicy foods
• Harsh skincare ingredients
Understanding personal triggers—and avoiding them—can be one of the most effective ways to manage the condition.
What This Means for Skincare
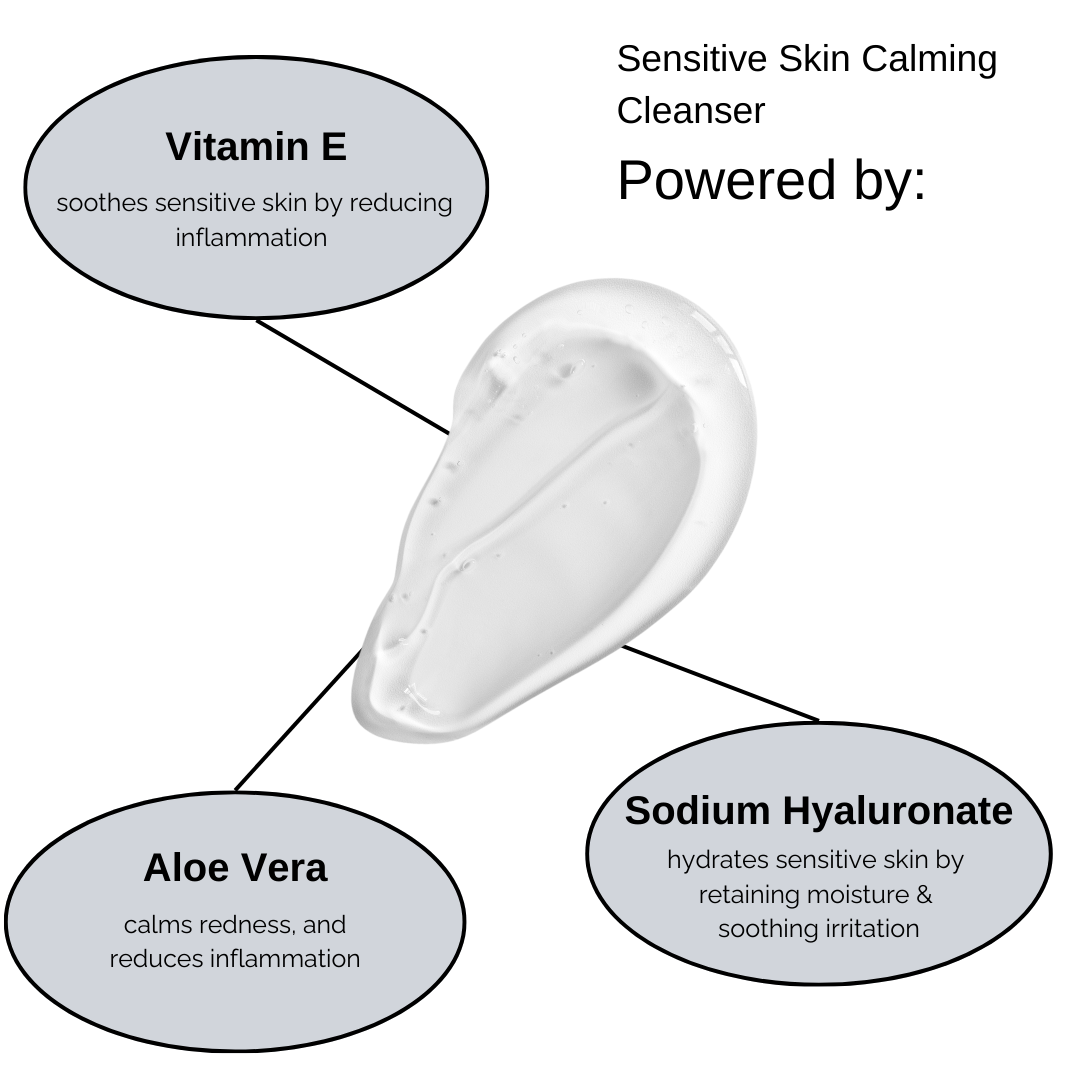
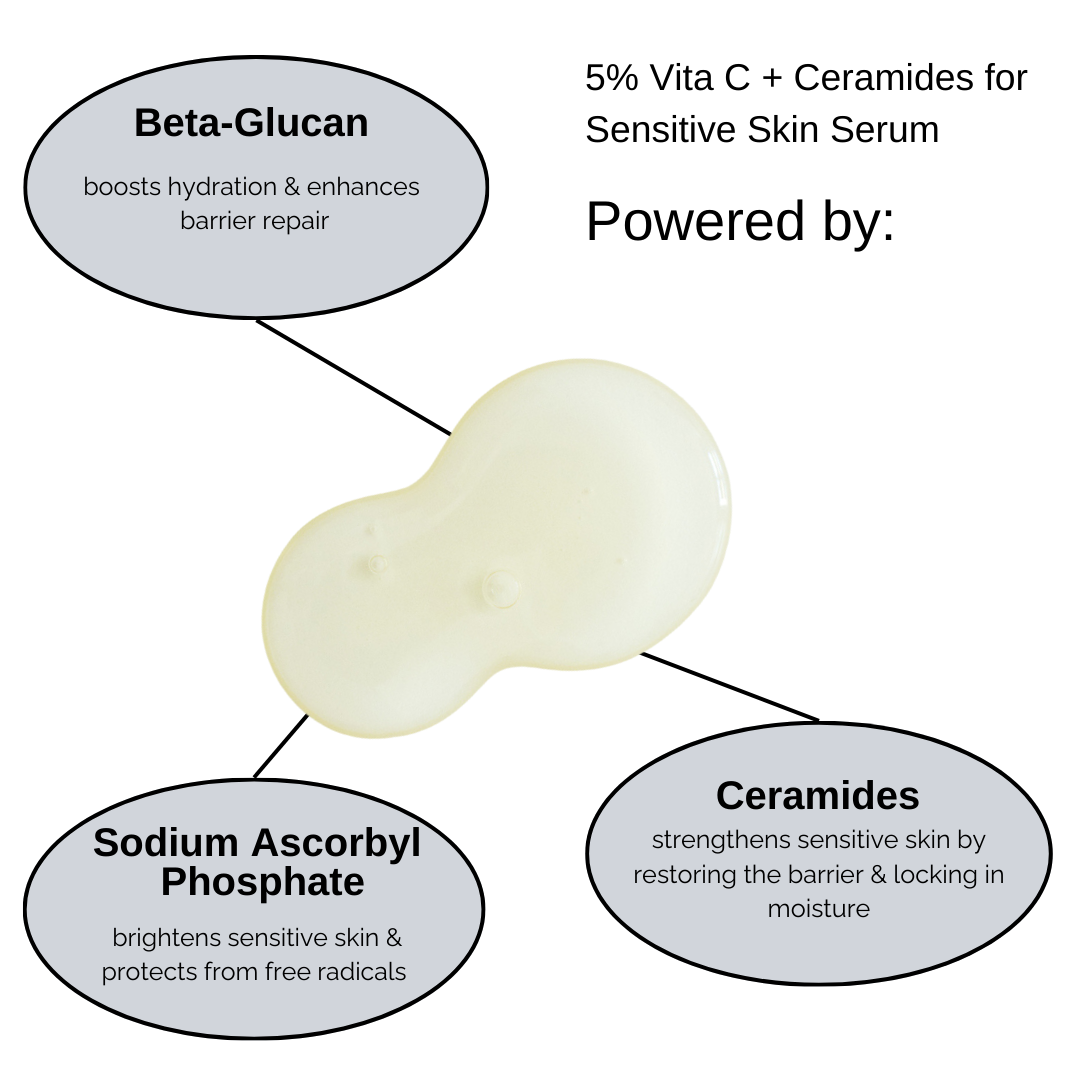
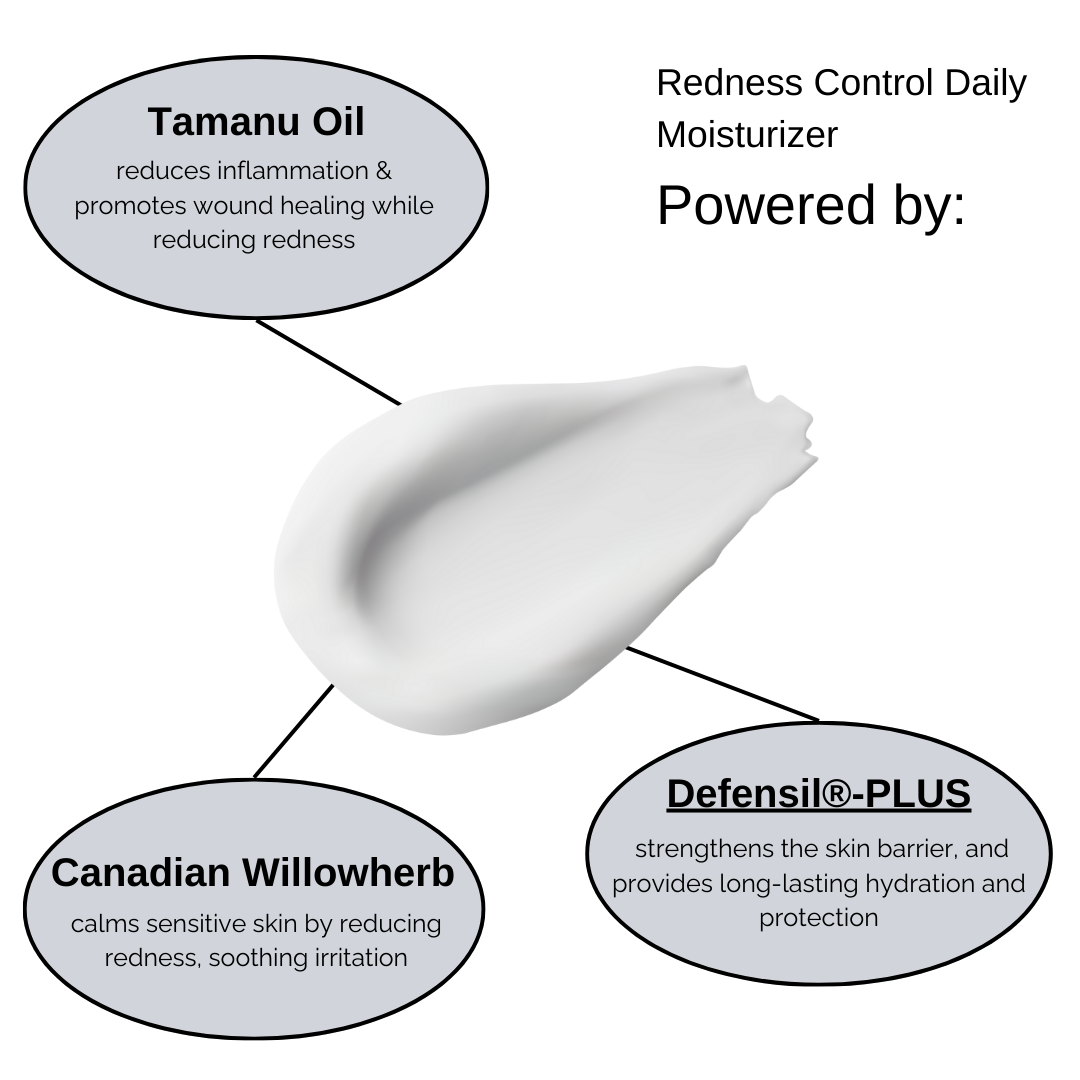
Understanding the complexity of rosacea reinforces the importance of gentle, barrier-supporting skincare that reduces inflammation and helps restore microbial balance. At RUDDI, we focus on formulating products that are:
• Fragrance-free
• pH-balanced
• Rich in anti-inflammatory and microbiome-friendly ingredients like azelaic acid, tamanu oil, and green tea extract
• pH-balanced
• Rich in anti-inflammatory and microbiome-friendly ingredients like azelaic acid, tamanu oil, and green tea extract
Looking Ahead: Future Therapies
Ongoing research is opening new doors:
• IL-17 inhibitors, currently used in psoriasis, are being studied for rosacea.
• Glutamate receptor modulators could target neurogenic inflammation.
• Microbiome therapies may offer personalized skin flora rebalancing.
As we continue to learn more about the root causes, future treatments may become even more effective—and tailored to your unique skin biology.